HemeHub
Committed to Hematology
A leading resource for advancing care and knowledge in hematological disorders. We provide case-based learning resources, targeted training, conference insights, and case reviews, connecting professionals and trainees with top experts in hematology.
Upcoming Live Webinars
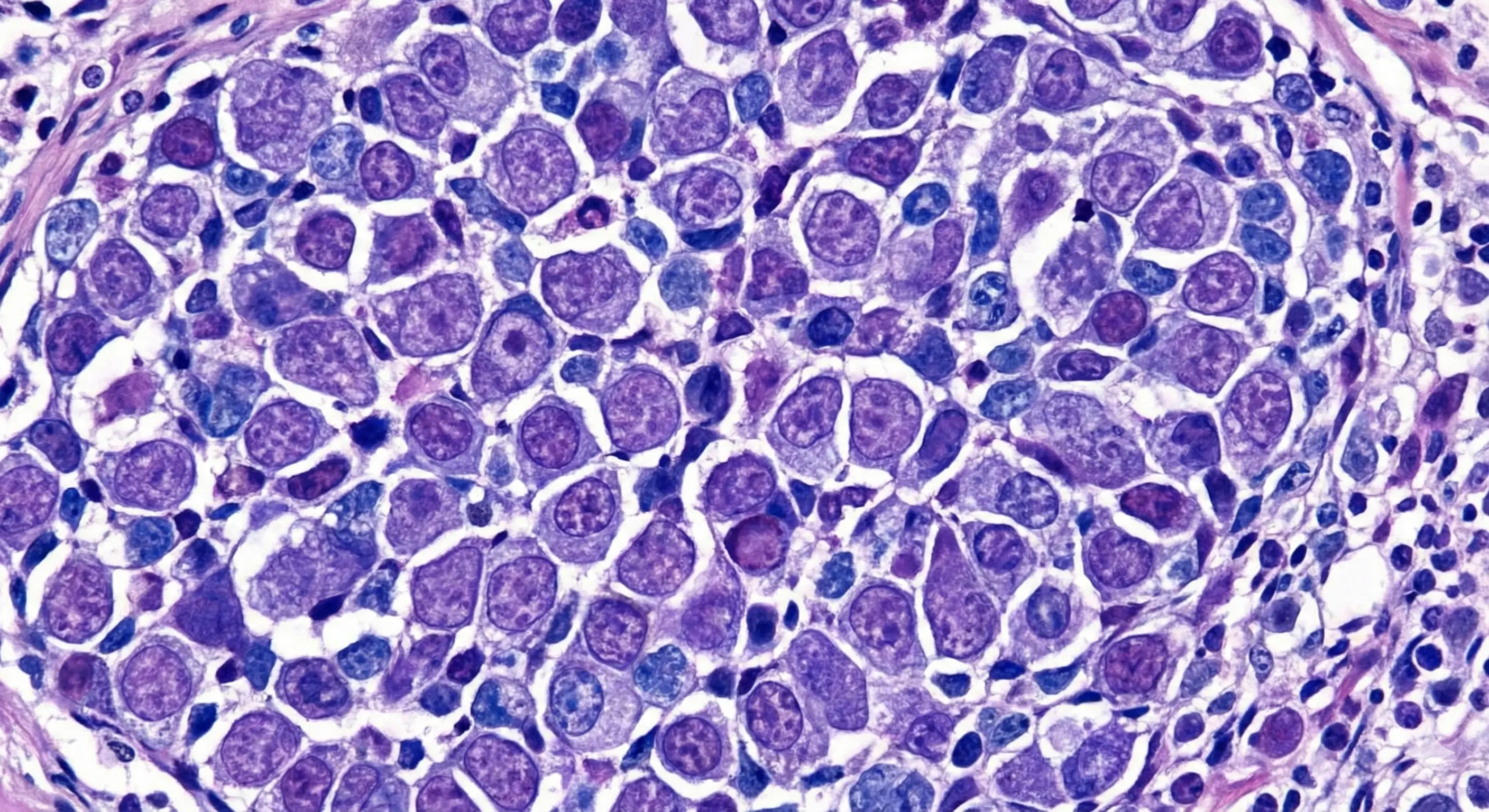
Ayalew Tefferi, MD is a professor of Hematology and Medicine at Mayo Clinic and a distinguished physician specializing in the pathophysiology, natural history, and treatment of chronic myeloproliferative neoplasms (MPNs), including polycythemia vera, essential thrombocythemia, and primary myelofibrosis. He completed his MD at the University of Athens Medical School, followed by a residency in internal medicine at St. Joseph Hospital in Chicago, IL. Ayalew Tefferi, MD then completed his residency in hematology and fellowship in hematology at the Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic College of Medicine and Science. His research encompasses both database and laboratory-based studies, aiming to develop new therapeutic drugs for these conditions. Ayalew Tefferi, MD meticulously analyzes clinical and laboratory risk factors predictive of patient outcomes in MPNs, such as fibrotic transformation, leukemic transformation, and overall survival. He utilizes disease-specific clinical databases, with data collected over several decades, to identify these risk factors. Additionally, he has led extensive research in genetic and mutational profiling of MPNs, resulting in the creation of genetic and clinical-molecular prognostic models, which are now integral to contemporary clinical care for patients with MPNs. He has spearheaded numerous clinical trials, contributing to the licensing of several drugs for MPNs in the U.S. Notable therapeutic agents include ruxolitinib and momelotinib for the treatment of myelofibrosis. Ayalew Tefferi, MD has also conducted pioneering studies on rare MPNs, including systemic mastocytosis, eosinophilic conditions, histiocytic disorders, and hemophagocytic lymphohistiocytosis. Chronic myeloproliferative neoplasms are a group of relatively uncommon diseases with poorly understood clinical and biological features, and the only curative treatment is stem cell transplantation. Ayalew Tefferi, MD's research has significantly enhanced the understanding of these diseases, identified critical patient characteristics, and developed new treatments. His work is widely adopted by MPN experts and incorporated into international guidelines. His studies on rare MPNs have also advanced disease biology understanding and informed rational treatment strategies. Ayalew Tefferi, MD is deeply committed to improving patient care by educating other healthcare professionals and sharing his extensive knowledge and expertise in the field of hematology.
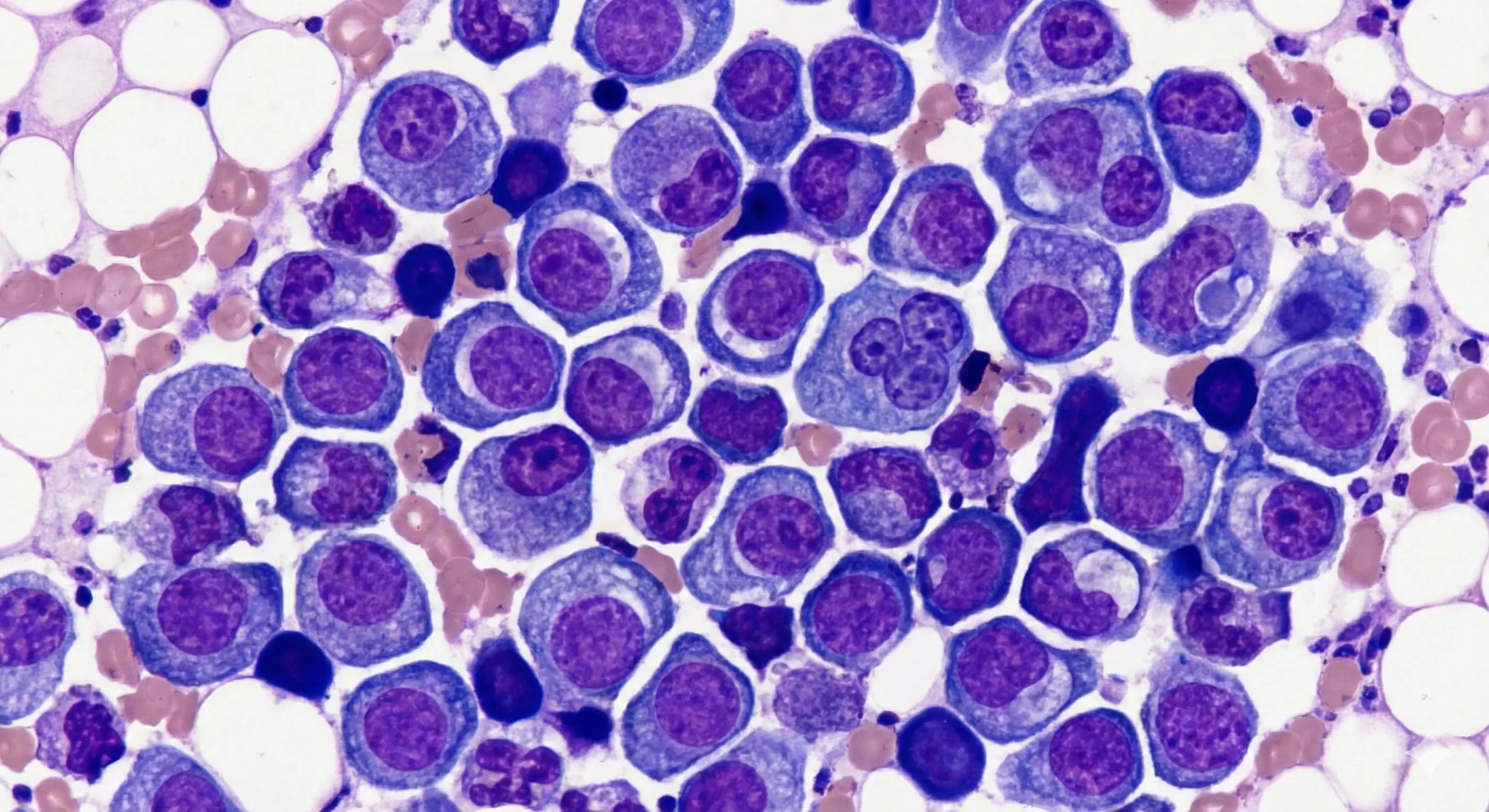
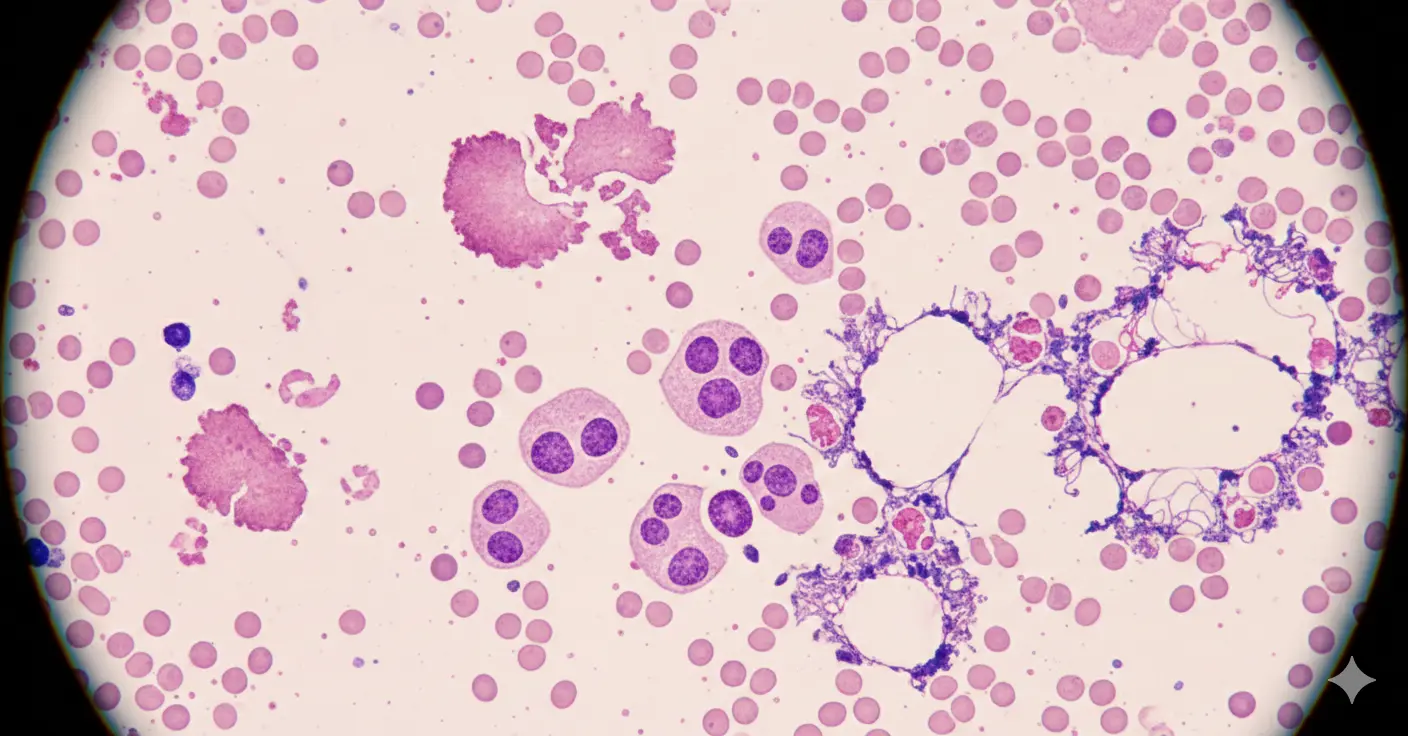
Mrinal S. Patnaik, MBBS is a physician scientist in the Division of Hematology within the Department of Internal Medicine at Mayo Clinic in Rochester, Minnesota. He serves as Chair of the Acute Leukemia and Myeloid Neoplasms Group in Rochester and is the Scientific Director of the Epigenetics Developmental Laboratory and the Epigenomics Program. He is actively involved in the Mayo Clinic Comprehensive Cancer Center and the Bone Marrow Transplant Program. Dr. Patnaik’s clinical and research expertise centers on precision genomics and epigenetics, with a focus on myeloid neoplasms and bone marrow failure syndromes. He directs the Mayo Clinic Clonal Hematopoiesis Clinic, the Bone Marrow Failure Syndrome Clinic, and the Short Telomere Clinic. His primary clinical interests include chronic myelomonocytic leukemia, myelodysplastic syndromes, myeloproliferative neoplasms, hereditary predisposition syndromes, and short telomere syndromes. He performs allogeneic stem cell transplantation and integrates genomic risk stratification into therapeutic decision making. Board certified in internal medicine and hematology by the American Board of Internal Medicine, Dr. Patnaik completed his residency and hematology oncology fellowship training at Mayo Clinic. He is recognized for excellence in education and mentorship, including induction into the Mayo Fellows Association Teacher of the Year Hall of Fame and receipt of the Internal Medicine Residents Outstanding Teaching Award. This session will provide a comprehensive clinical update in chronic myelomonocytic leukemia, highlighting key aspects of diagnosis, risk assessment, and current treatment approaches. Emphasis will be placed on practical management strategies, evolving therapeutic options, and individualized patient care to support informed decision making in the management of CMML.
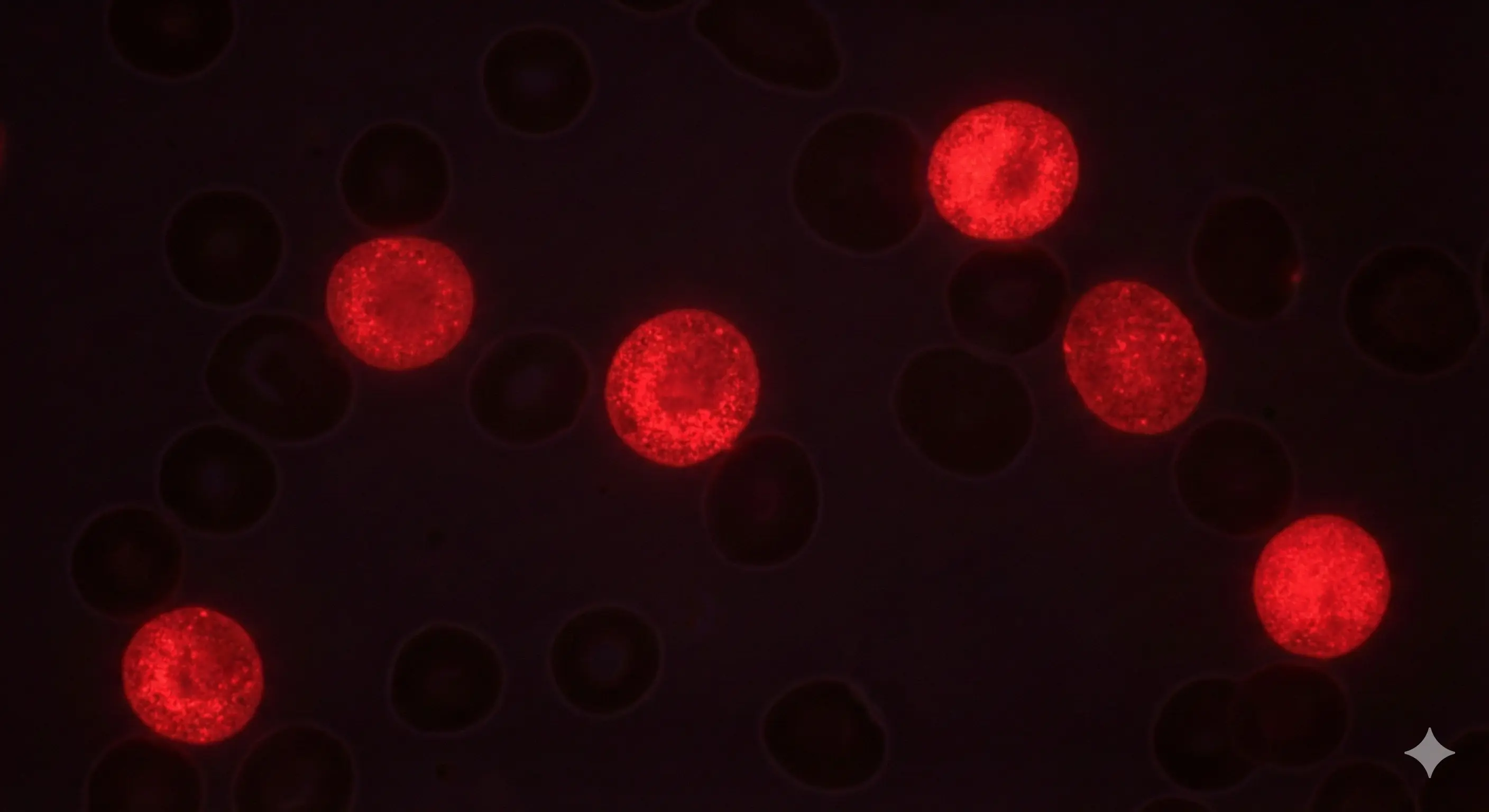
Ilene Weitz, MD is a Professor of Clinical Medicine at the Keck School of Medicine at the University of Southern California (USC). She practices at LAC+USC Medical Center, Keck Hospital of USC, and USC Norris Cancer Hospital. Ilene Weitz, MD is board-certified in Internal Medicine and Hematology. She earned her medical degree from the Medical College of Pennsylvania in Philadelphia, completed her internship and residency in internal medicine at Cedars-Sinai Medical Center, and pursued a fellowship in hematology/oncology at Scripps Clinic and Research Foundation in La Jolla, California. Ilene Weitz, MD's clinical and research interests encompass a range of hematologic disorders, including paroxysmal nocturnal hemoglobinuria (PNH), atypical hemolytic uremic syndrome (aHUS), cold agglutinin disease, thrombotic microangiopathies (TMA), sickle cell disease, thalassemia, and immune-mediated anemias and thrombocytopenia. She has contributed to numerous publications in journals such as the American Journal of Hematology, Journal of Clinical Oncology, and Hepatology, and has authored several book chapters and reviews. A dedicated educator, Ilene Weitz, MD has been recognized with the Morris Press Humanism Award and the Golden Apple Outstanding Physician Educator Award from Cedars-Sinai Medical Center. She has also received the Outstanding Voluntary Faculty Award in the Division of Hematology from USC School of Medicine. Ilene Weitz, MD continues to advance the field of hematology through her clinical practice, research, and commitment to medical education.
Upcoming Hybrid Events

HemeHub
Hematology Summit
A premier gathering of minds delivering the latest clinical updates and actionable guidance for the management of complex hematologic diseases.
Location
Dallas–Fort Worth, Texas
Date
October 3, 2026


Live Webinars
Join live case discussions and expert sessions with leading hematology professionals worldwide.

Group Specific Education
Access tailored training programs and educational content designed for different professional groups.

Scientific Conference Calendar
Stay informed about upcoming hematology conferences worldwide with key dates and submission deadlines.
Latest Live Webinars

POST ASH 2025 Updates
In this post-ASH 2025 discussion, Musa Yilmaz, Elif Yilmaz, Adeel Khan, and Taha Bat collectively review major updates from the 2025 American Society of Hematology Annual Meeting, focusing on findings with the greatest relevance to current and future clinical practice in myeloid, marrow failure, lymphoma and myeloma disorders. The speakers synthesize emerging data across hematologic malignancies and bone marrow failure syndromes, highlighting evolving treatment approaches and the growing role of novel and targeted therapies. Throughout the session, each presenter contributes expert perspective on how recent trial results and therapeutic advances may influence real-world decision-making. By emphasizing broader trends—such as personalization of therapy, integration of innovative agents, and thoughtful translation of research into practice—the discussion provides a cohesive and forward-looking overview of where the field of hematology is heading, while identifying ongoing challenges and areas of unmet need.

Hemophilia A
In this session, Shannon Meeks, MD, and Ibrahim Ibrahim, MD review current best practices for managing Hemophilia A. They emphasize the move toward individualized, preventive care, noting that well-designed prophylactic therapycan significantly reduce bleeding events and prevent long-term joint damage. The speakers highlight the ongoing need to monitor for complications, particularly inhibitor development and joint deterioration, even with modern treatments. They also stress that optimal outcomes depend on multidisciplinary care, integrating hematology, nursing, physical therapy, and patient-education support to address both clinical and psychosocial needs.
Sickle Cell Disease and Gene Therapy
In this session, Thomas Coates, MD and Ibrahim Ibrahim, MD provide an in-depth discussion about the state of gene therapy for sickle cell disease. They outline how gene therapy — by genetically correcting or ameliorating the mutation responsible for SCD in hematopoietic (blood-forming) stem cells — is transitioning from theoretical to actual clinical application. They caution, however, that while gene therapy offers hope for a “cure,” it's not a magic bullet. Concerns remain around long-term safety, durability of therapeutic effects, and equitable access. The speakers stress that even after gene therapy, patients may still require traditional supportive care and monitoring for complications. Finally, they call for strong research infrastructure — including long-term follow-up studies, registries, and multidisciplinary care teams — as critical to properly evaluate and deliver gene therapies to SCD patients.
Upcoming Scientific Conferences
Hemostasis & Thrombosis Research Society (HTRS) 2026 Scientific Symposium
A global event for experts in thrombosis, hemostasis, and vascular biology, featuring plenaries, workshops, and networking opportunities.
British Society for Haematology (BSH) 66th Annual Scientific Meeting
The BSH 66th Annual Scientific Meeting is a key event for hematology professionals, providing the latest research and clinical advances in hematology. It offers educational sessions, networking opportunities, and discussions on the management of hematological conditions.
American Society of Pediatric Hematology/Oncology (ASPHO) Conference
An annual conference dedicated to pediatric hematology and oncology, offering educational sessions, research presentations, and networking opportunities for professionals.